New study reveals brain mechanisms involved in genetically based autism which may lead to effective treatment
A groundbreaking study from Tel Aviv University expands the understanding of the biological mechanism underlying genetically-based autism, specifically mutations in the SHANK3gene, responsible for nearly one million cases of autism worldwide. Based on these discoveries, the research team applied a genetic treatment that improved the function of cells affected by the mutation, laying a foundation for future treatments for SHANK3-related autism.
The study was led by the lab of Prof. Boaz Barak and PhD student Inbar Fischer from the Sagol School of Neuroscience and the School of Psychological Sciences at Tel Aviv University, in collaboration with the labs of Prof. Ben Maoz from the Department of Biomedical Engineering at Fleischman Faculty of Engineering at Tel Aviv University and Prof. Shani Stern from the Department of Neurobiology at the University of Haifa. The article was published in the prestigious journal Science Advances.
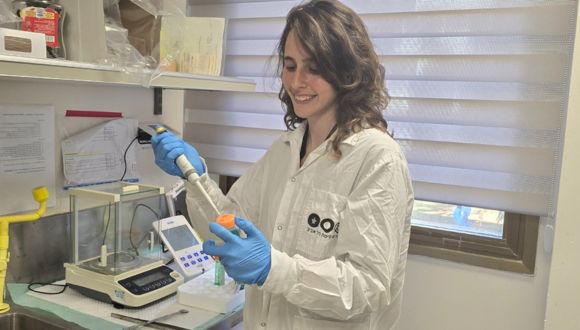
PhD student Inbar Fischer.
Prof. Barak: “Autism is a relatively common neurodevelopmental disorder. According to current data, 1-2% of the global population and one in every 36 boys in the U.S. are diagnosed with autism spectrum disorder (ASD), with numbers rising over time. Autism is caused by a wide range of factors – environmental, genetic, and even social and cultural (such as the rise in parental age at conception). In my lab, we study the genetic causes of autism. Among these are mutations in a gene called SHANK3. The impact of these mutations on the function of brain neurons has been extensively studied, and we know that the protein encoded by SHANK3 plays a central role in binding receptors in the neuron, essential for receiving chemical signals (neurotransmitters and others) by which neurons communicate. Thus, damage to this gene can disrupt message transmission between neurons, impairing the brain’s development and function. In this study we sought to shed light on other, previously unknown mechanisms, through which mutations in the SHANK3 gene disrupt brain development, leading to disorders manifested as autism”.
Specifically, the research team focused on two components in the brain that have not yet been studied extensively in this context: non-neuronal brain cells (glia) called oligodendrocytes and the myelin they produce. Myelin tissue is a fatty layer that insulates nerve fibers (axons), similar to the insulating layer that coats electrical cables. When the myelin is faulty, the electrical signals transmitted through the axons may leak, disrupting the message transmission between brain regions and impairing brain function.
How a Gene Mutation Impacts the Brain
The team employed a genetically engineered mouse model for autism, introducing a mutation in the Shank3 gene that mirrors the mutation found in humans with this form of autism. Inbar Fischer: “Through this model, we found that the mutation causes a dual impairment in the brain’s development and proper function: first, in oligodendrocytes, as in neurons, the SHANK3 protein is essential for the binding and functioning of receptors that receive chemical signals (neurotransmitters and others) from neighboring cells. This means that the defective protein associated with autism disrupts message transmission to these vital support cells. Secondly, when the function and development of oligodendrocytes is impaired, their myelin production is also disrupted. The faulty myelin does not properly insulate the neuron’s axons, thereby reducing the efficiency of electrical signal transmission between brain cells, as well as the synchronization of electrical activity between different parts of the brain. In our model, we found myelin impairment in multiple brain areas and observed that the animals’ behavior was adversely affected as a result”.
The researchers then sought a method for fixing the damage caused by the mutation, with the hope of ultimately developing a treatment for humans. Inbar Fischer: “We obtained oligodendrocytes from the brain of a mouse with a Shank3 mutation, and inserted DNA segments containing the normal human SHANK3 sequence. Our goal was to allow the normal gene to encode a functional and normal protein, which, replacing the defective protein, would perform its essential role in the cell. To our delight, following treatment, the cells expressed the normal SHANK3 protein, enabling the construction of a functional protein substrate to bind the receptors that receive electrical signals. In other words, the genetic treatment we had developed repaired the oligodendrocytes’ communication sites, essential for the cells’ proper development and function as myelin producers”.
To validate findings from the mouse model, the research team generated induced pluripotent stem cells from the skin cells of a girl with autism caused by a SHANK3 gene mutation identical to that in the mice. From these stem cells, they derived human oligodendrocytes with the same genetic profile. These oligodendrocytes displayed impairments similar to those observed in their mouse counterparts.
Autism and Myelin Damage: New Hope for Treatment
Prof. Barak concludes: “In our study, we discovered two new brain mechanisms involved in genetically induced autism: damage to oligodendrocytes and, consequently, damage to the myelin they produce. These findings have important implications – both clinical and scientific. Scientifically, we learned that defective myelin plays a significant role in autism and identified the mechanism causing the damage to myelin. Additionally, we revealed a new role for the SHANK3 protein: building and maintaining a functional binding substrate for receptors critical for message reception in oligodendrocytes (not just in neurons). We discovered that contrary to the prevailing view, these cells play essential roles in their own right, far beyond the support they provide for neurons — often seen as the main players in the brain. In the clinical sphere, we validated a gene therapy approach that led to significantly improved development and function of oligodendrocytes derived from the brains of mice modeling autism. This finding offers hope for developing genetic treatment for humans, which could improve the myelin production process in the brain. Furthermore, recognizing the significance of myelin impairment in autism—whether linked to the SHANK3 gene or not—opens new pathways for understanding the brain mechanisms underlying autism and paves the way for future treatment development”.