TAU Researchers discovered a potential new target for developing effective treatments for Parkinson’s disease.
Researchers at Tel Aviv University discovered a new factor in the pathology of Parkinson’s disease, which in the future may serve as a target for developing new treatments for this terrible ailment, affecting close to 10 million people worldwide.
The researchers: “We found that a variant of the TMEM16F protein, caused by a genetic mutation, enhances the spread of Parkinson’s pathology through nerve cells in the brain”.
The study was led by Dr. Avraham Ashkenazi and PhD student Stav Cohen Adiv Mordechai from the Department of Cell and Developmental Biology at TAU’s Faculty of Medical and Health Sciences and the Sagol School of Neuroscience. Other contributors included: Dr. Orly Goldstein, Prof. Avi Orr-Urtreger, Prof. Tanya Gurevich and Prof. Nir Giladi from TAU’s Faculty of Medical and Health Sciences and the Tel Aviv Sourasky Medical Center, as well as other researchers from TAU and the University of Haifa. The study was backed by the Aufzien Family Center for the Prevention and Treatment of Parkinson’s Disease at TAU. The paper was published in the scientific journal Aging Cell.
Doctoral student Stav Cohen Adiv Mordechai explains: “A key mechanism of Parkinson’s disease is the aggregation in brain cells of the protein α-synuclein (in the form of Lewy bodies), eventually killing these cells. For many years, researchers have tried to discover how the pathological version of α-synuclein spreads through the brain, affecting one cell after another, and gradually destroying whole brain sections. Since α-synuclein needs to cross the cell membrane to spread, we focused on the protein TMEM16F, a regulator situated in the cell membrane, as a possible driver of this lethal process”.
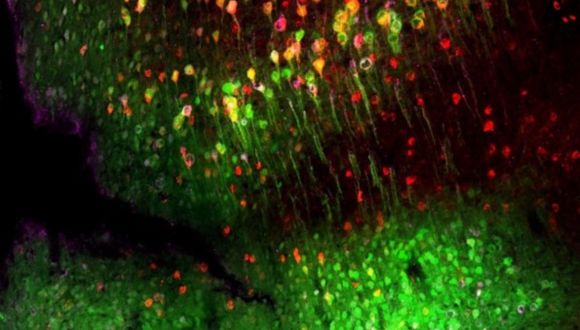
α-synuclein spread in the mouse brain.
At first, the researchers genetically engineered a mouse model without the TMEM16F gene, and derived neurons from the brains of these mice for an in-vitro cellular model. Using a specially engineered virus, they caused these neurons to express the defective α-synuclein associated with Parkinson’s and compared the results with outcomes from normal brain cells containing TMEM16F. They found that when the TMEM16F gene had been deleted, the α-synuclein pathology spread to fewer healthy neighboring cells compared to the spread from normal cells. The results were validated in-vivo in a living mouse model of Parkinson’s disease.
TMEM16F Mutation Linked to Parkinson’s Risk in Ashkenazi Jews
In addition, in collaboration with the Neurological Institute at the Tel Aviv Sourasky Medical Center, the researchers looked for mutations (variants) in the TMEM16F gene that might increase the risk for Parkinson’s disease. Dr. Ashkenazi explains: “The incidence of Parkinson’s among Ashkenazi Jews is known to be relatively high, and the Institute conducts a vast ongoing genetic study on Ashkenazi Jews who carry genes increasing the risk for the disease. With their help, we were able to identify a specific TMEM16F mutation which is common in Ashkenazi Jews in general, and in Ashkenazi Parkinson’s patients in particular”. Cells carrying the mutation were found to secrete more pathological α-synuclein compared to cells with the normal gene. The researchers explain that the mechanism behind increased secretion has to do with the biological function of the TMEM16F protein: the mutation increases the activity of TMEM16F, thereby affecting membrane secretion processes.
Stav Cohen Adiv Mordechai: “In our study, we discovered a new factor underlying Parkinson’s disease: the protein TMEM16F, which mediates secretion of the pathological α-synuclein protein through the cell membrane to the cell environment. Picked up by healthy neurons nearby, the defective α-synuclein forms Lewy bodies inside them, and gradually spreads through the brain, damaging more and more brain cells. Our findings mark TMEM16F as a possible new target for the development of effective treatments for Parkinson’s disease. If, by inhibiting TMEM16F, we can stop or reduce the secretion of defective α-synuclein from brain cells, we may be able to slow down or even halt the spread of the disease through the brain”.
Dr. Ashkenazi emphasizes that research on the new Parkinson’s mechanism has only begun, and quite a number of questions still remain to be explored: Does inhibiting TMEM16F actually reduce the symptoms of Parkinson’s disease? Does the lipid composition of cell membranes play a part in spreading the disease in the brain? Is there a link between mutations in TMEM16F and the prevalence of Parkinson’s in the population? The research team intends to continue the investigation in these directions and more.